Category Archives: Uncategorized
Music and Baby Development
Another Reason to Turn Off the TV and Turn On the Music!
Babies love to share music with others. They use sounds, movements and expressions to interact with others and connect with their own feelings. Music often becomes the first form of creative expression for infants and toddlers. It can also give them a way to connect and bond with the caregivers around them. Music can also be a powerful way to connect babies to their own heritage or culture or another language.
Music has so many developmental benefits. There is no doubt that babies and young children seem to love music, but what are they really getting out of it? What does dancing, bouncing and clapping really have to do with development?
Familiar, soothing sounds.
Many parents play an instrument or sing to their babies long before they are born and some babies respond to music played to them in utero by becoming more active. Infants also can recognize songs or sounds familiar from pregnancy, and make a distinction between a song that a mother sang during her pregnancy, and one that they have never heard before.
Young children are attracted to musical patterns and structure. Research has shown that music helps children build early mathematical skills by teaching spatial properties, one-to-one correspondence, sequencing, patterning and early counting. Babies seem to have a natural affinity for rhythm. Babies follow the beat of music playing and move their body to the tempo naturally when parents sing to them.
Benefits of steady beat. Patting the beat of a song on your baby’s legs, or bouncing to music rhythmically helps your baby “feel” the steady beat. Steady beat also has similar brain relationships to the coordination needed for other rhythmic skills like marching and running.
Finger Plays help fine motor skills. Infants and toddlers learn imitation, fine motor and language skills through the hand motions that accompany many songs for young children. Most songs we sing with infants and toddler include clapping at the end of songs or special finger plays for special parts, like the mama duck quacking in “Five Little Ducks” or the wheels turning on “The Wheels on the Bus.”
Language Development. As older babies begin experiencing rapid language growth and their ability to distinguish between spoken sounds exponentially increases, so does their ability to distinguish between musical sounds, note and tones of instruments. Music development and language development support each other and support the baby’s sense of making himself understood in the world.
Feel the Music! Music is an outlet for energy, emotions and creativity. Music can be joyful and exciting, and it is impossible to sing silly songs to a child without a smile on your face. Music can also be soothing and calming, like a lullaby that is shared at the end of the day, or the tender humming while walking a newborn to sleep.
Music helps to establish routines and transitions. A familiar song will help a baby feel safe and secure in an unfamiliar setting, just like a lovey or familiar toy. Music plays an important role in establishing routines. The same song for bedtime becomes part of the transition from awake to drowsy, or a clean-up song becomes the transition from playing to tidying up for dinner.
Bronchiolitis and Croup
Bronchiolitis: A common respiratory illness during a baby’s first year
Your baby will (unfortunately) contract six colds, on average, during his first year. Most colds will have upper respiratory symptoms (runny or stuffy nose, perhaps a cough, possibly a fever). Most colds will last for 5-10 days (yes, it takes longer for babies to shake a cold than an adult. Also, the baby’s symptoms are much more obvious since they cannot blow their nose, and they let you know when they are not feeling their best).
Occasionally, some colds have a “Stage Two” attached.
There are three common “Stage Two” parts of colds: some babies will get an ear infection after a cold (due to physiologic anatomy and nasal congestion), some cold viruses will result in a body rash (“viral rash”) one or two weeks after the cold virus has resolved, and finally, some colds will travel lower in the baby’s respiratory tract and continue on into a Croup or Bronchiolitis. Croup is more common in 1-2 year olds. Bronchiolitis is more common during a baby’s first year.
So, think of bronchiolitis as “part two” of a cold. The cold virus unfortunately has moved lower in the baby’s respiratory tract, to the smallest of the airway branches, called the bronchioles. An adult typically gets “bronchitis” from a chest cold (inflammation of the bronchi), but an infant gets “bronchiolitis” – inflammation of the smaller branches of the respiratory system.
These respiratory infections are unique in that they typically impact infants and toddlers, but not adults. However, the very same virus that may cause a basic cold in anyone, a “head cold” or “chest cold” for others in the home, may result in croup or bronchiolitis in an infant or toddler. It’s not the virus itself that causes the bronchiolitis (or croup, or ear infection), rather, the virus causes the infection, and the infection progresses to a symptom in the bronchioles (or middle ear).
Bronchiolitis is an infection of the respiratory tract that affects the smallest airways of the lung. The swelling and obstruction of these tiny airway passages creates shortness of breath, wheezing or whistling noises. You might notices an infant with bronchiolitis is working harder, with rapid, shallow breathing, with neck or chest “accessory muscles” moving with the breathing efforts. You’ll likely notice more irritability or crankiness, restlessness and decreased appetite as the body’s efforts must go into breathing and oxygenation rather than eating and nutrition.
Since the virus that causes bronchiolitis is often the same virus that causes the common cold, you may see cold symptoms including a runny or stuffy nose, cough and fever. Bronchiolitis or croup may start with a common cold, but progress to the lower respiratory tract.
Even if your baby doesn’t seem to be struggling to breathe, restlessness may be a sign of low oxygen levels in an infant, so it’s worth a call to your pediatrician if your baby has a fever, congestion, is breathing rapidly and seems very unsettled or unhappy. It’s better to call and be told what to watch for, than worry about if you should call or not!
Bronchiolitis is most common in the winter and spring but may occur at any time. It is most common in babies under a year old, boys are more commonly affected and exposure to smoke, daycare or older siblings makes a baby more likely to get more frequent colds, so also increase the risk or rate of bronchiolitis. Avoiding obviously sick people (hard to do in daycare where seemingly 75% of children appear to have some stage of a cold!) and good hand washing are always good practices to reduce risk of catching a cold or virus.
RSV (respiratory syncytial virus) is the most common viral cause of bronchiolitis (though the flu virus or a regular rhinovirus – the common cold virus – may also result in bronchiolitis in an infant). Premature and other vulnerable infants are more susceptible to RSV, or may have a harder time managing RSV illnesses, so some higher-risk babies may receive a vaccine to prevent RSV.
Your pediatrician will diagnose bronchiolitis by listening to your baby’s chest, checking a pulse oximetry oxygen level and perhaps ruling out pneumonia or another diagnosis by requesting a chest x-ray. Presense of the RSV virus may be confirmed using a nasal swab in the pediatrician’s office.
Treatment for bronchiolitis will depend on your baby’s specific symptoms and severity. Most bronchiolitis cases are mild and will be cared for at home by offering fluids, anti-fever medications, and using a humidifier and saline nose drops to keep breathing more comfortable. Occasionally “nebulizer” breathing treatments may be done in the doctor’s office or at home. Rarely, a baby may need to be briefly hospitalized for breathing treatments or extra oxygen but this is not typical at all. Antibiotics will not help bronchiolitis, which is the infant’s respiratory response to a virus similar to a cold.
Protected: Reading
Protected: Pedi and OB Referrals
Protected: Lou
Protected: References
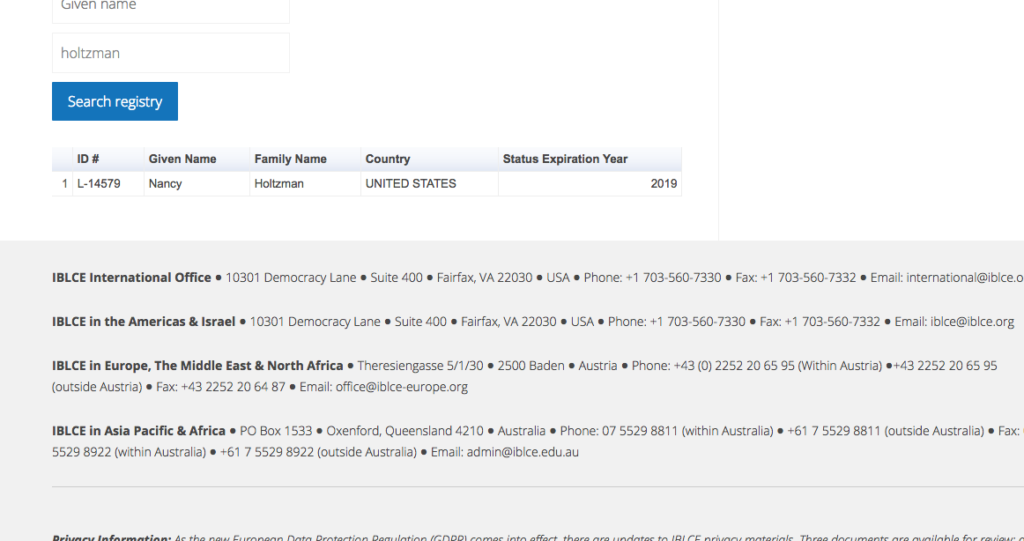
IBCLC Certification Verification
Below is a screenshot. To check my credential yourself, visit
https://iblce.org/public-registry/
Enter Holtzman as “family name” and Nancy as “given name”.
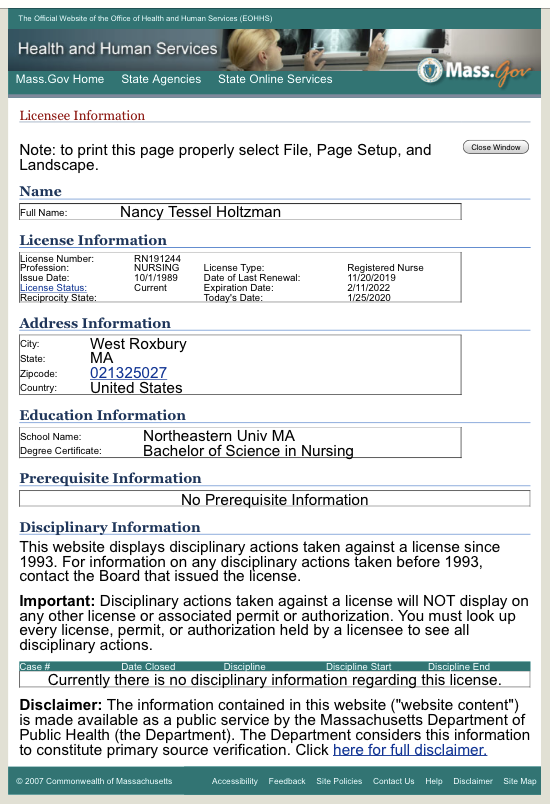
RN License verification
Below is a screenshot.
If you’d like to do the search yourself, visit the
Health and Human Services registry
and enter RN191244 and/or Nancy Holtzman for easiest access on a clunky search system.
Links and such
(This may look like a random collection of links to most. That’s ok, feel free to click and enjoy)
History, Legacy, Feel-Good Stuff:
Great Beginnings New Mothers Groups. My Legacy. Begun in West Roxbury, 1995. Ended in 2014, after reaching 25,000 families in five states and thirteen locations. The curriculum is continued in a variety of community centers, childcare programs, birth centers and parenting programs nationally. See the experiences of some original Isis participants.
Magic Beans says a thoughtful Goodbye to Isis Parenting and Nancy
The Atlantic covers the MIT Program Building a Better Breastpump
Boston Globe’s thoughts on What Happened to Isis. (they only get it half-right, but it’s still nice)
Journal of Obstetric, GYN and Neonatal Nursing (JOGNN) free access to my publication abstract on Early Parenting and Sleep.
AWHONN (Association of Women’s Health, Obstetric and Neonatal Nurses) see my Super Cool Sleep Poster presentation on supporting parents around infant sleep.
Links Related to Topics Discussed
Go on, take a bath together! Newborn Co-Bathing is a thing if your baby hates the baby tub.
Brief Pump, Store and Feed Careplan may be useful. More on this later.
Breastfeeding Webinar Five Tips for Better Pumping with info about why I recommend pumping after breastfeeding, not mid-way between feeds.
How to Nurse Sidelying and on both sides! Best tweaked in person – remind me.
Soon less crying, more playing on the Changing Table! I promise!
Cradle Cap from Mayo Clinic (a trustworthy clinical source for parents IMO) – we can discuss if you want to use Head’n’Shoulders ( if pedi-approved) and get rid of it in a week, or nothing or jojoba or coconut oil and get rid of it in 1-2 months. Either way works.
How to SAVE a Baby’s LIFE – INFANT CPR ! Watch this 3 min. video. Also, a 2 minute choke-saving skills video review. Let’s review both of these important skills!
For S.: my favorite Infant Massage music – the original House at Pooh Corner. We also talked about Tummy Massage for Gas.
Verify Credentials: RN CPN IBCLC
RN: View my Registered Nursing License here, current and in good standing since 1989. That’s 30 years if you are sleep deprived 😉 Check credentials.
CPN: View my Board Certification for Pediatric Nursing here, an advanced credential held for a decade and recertified every two years. View verification
IBCLC: International Board Certified Lactation Consultant – in continuous practice since 1998. Yes, I have been a BOARD CERTIFIED feeding specialist for over 20 years, learning more each week from every mom and baby I meet. Verify IBCLC credential